
Severe Varicose Veins
Venous disease is a progressive condition. It will not improve or go away by itself. As time passes, there will be an increasing number of varicose veins, spider veins, and other painful symptoms that will worsen too. It can develop into the breakdown of the skin, open sores that won’t heal, and even blood clots.
What are the symptoms of severe varicose veins / chronic venous disease?
Patients with severe venous disease may have signs such as venous eczema (venous dermatitis), swelling in the leg (oedema), discolouration of the skin (hyperpigmentation), thickening of the skin of the lower leg or ankle (lipodermatosclerosis), and localised or extensive break downs of the skin barrier, particularly around the ankle region (venous ulceration.) As well as this, patients can experience heaviness, aching and tiredness in the legs. If left untreated, these symptoms are likely to become worse with advancing age.
Lipodermatosclerosis can greatly affect the health of the lower leg and lead to complications such as severe inflammation (phlebitis) and infection (cellulitis); varicose veins can form clots (thrombophlebitis) and venous ulcers can become quite troublesome and difficult to treat, particularly when they bleed, weep or become infected.
Symptoms and Complications of Severe Venous Disease
A brief description of each of the complications of untreated and progressive varicose veins or chronic venous disease.
Learn more about how phlebologists classify venous disease here.

Venous Eczema
Venous Eczema
(also known as , venous , or ) is where the surrounding the becomes scaly, red, and itchy. This can be mild and limited to the localised areas, or it can cover the whole , where the is very inflamed.
Symptoms of venous eczema
Near and ankles: dry scaly , itching, pain, open sores that ooze or crust due to scratching, thickened or rough .
What causes venous eczema?
When incompetent veins fail at returning blood to the heart, blood pools, and pressure build up inside the vein. This is known as venous hypertension (an increase in localised blood pressure). This additional pressure pushes blood into the capillaries, the tiny veins near the surface of the skin. Venous hypertension is the main cause of venous stasis dermatitis and inflammation in progressive venous disease.
With the increased pressure in the capillaries and blood vessels, red blood cells leak out close to the surface. The immune system sends inflammatory cells to the leaked red blood cells to start the healing process via a reaction in the . However, as the red blood cells continue to leak thanks to , the becomes chronic . The feels irritated, itchy, and the can break down and become rough, scaly, with sores forming because of the scratching. These open sores () can be difficult to heal until the underlying problem of the is dealt with. Until then, they can cause infections and be painful.

Hyperpigmentation
Hyperpigmentation – Discolouration of the skin
Hyperpigmentation is a typical sign of advancing venous disease. This is the development of skin discolouration above the ankle, often localised to a varicose vein. If blood flow leaks out of the damaged blood vessel, the haemoglobin breaks down and disperses in the tissue, this causes discolouration, known as hyperpigmentation.
Symptoms of hyperpigmentation
Brown staining of the skin surface near the ankle.
What causes hyperpigmentation?
When varicosities leak blood (including red blood cells and haemoglobin) into the capillaries and tissues near the surface of the skin, they are broken down into iron which stains the skin. This can become quite dark. When the underlying varicose veins are treated, the colour usually lightens somewhat, however, the staining may not completely disappear.
Hyperpigmentation can also occur after sclerotherapy treatment, read more about it here.

Oedema
Oedema – Swelling of the leg
Oedema is a complication of chronic venous disease where the ankle, foot, and/or lower leg swells. Swelling can sometimes occur in patients with less advanced varicose veins, but is often present in advanced cases of severe venous disease.

Venous Ulcer
Venous Ulcer – Open sores
Localised or extensive breakdown of the skin barrier, particularly around the ankle region. If left untreated, severe venous disease leads to worsening symptoms in the lower legs, which will ultimately culminate in the development of a venous ulcer. The ulcer may be small or large. Ulcer treatment can be complex and must be managed correctly, with a combination of conservative and medical interventions by a phlebologist.

Lipodermatosclerosis
Lipodermatosclerosis – Thickening of the skin of the lower leg or ankle
One of the stages of skin change prior to ulceration is referred to as lipodermatosclerosis or chronic panniculitis. The is a thickening of the skin and soft tissue in the lower leg and ankle primarily in association with chronic venous disease and varicose veins.
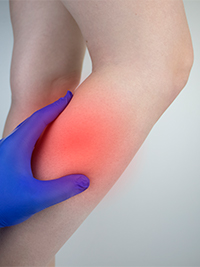
Phlebitis and Cellulitis
Severe bacterial infection of the vein and the surrounding tissues below the skin.

Thrombophlebitis
Thrombophlebitis
Thrombophlebitis is the inflammation and blood clotting of a vein. Blood clotting is a normal function that stops bleeding after an injury. When it happens within a vein and hinders blood flow, it can lead to serious health problems.
Symptoms of thrombophlebitis
Swelling, tenderness and the skin feels warm to the touch. However, many patients show no symptoms (asymptomatic).
The signs can be difficult to identify because of other conditions with similar symptoms, such as skin irritations, ruptured cysts, muscle strain, phlebitis, and cellulitis.
What causes thrombophlebitis?
Thrombophlebitis (inflammation and blood clot) occurs when the body mistakes the pooling of the blood in a varicose vein for blood loss. The body sends inflammatory cells and white blood cells to stop the ‘bleeding’. This clots the blood. As the clot occurs inside the vein, it can obstruct the free flow of blood.
The danger to health can depend on the location of the clot. If it forms in a vein close to the skin (superficial vein thrombosis), it can cause inflammation of nearby tissues, development of red lumps, and the whole limb can become swollen. If the clot occurs in a deeper vein (deep vein thrombosis), the clot can break off and travel to the heart and lungs, leading to a pulmonary embolism. This could be life-threatening.
How We Treat Severe Varicose Veins / Chronic Venous Disease
Ultrasound Guided Sclerotherapy
Ultrasound Guided Sclerotherapy is a highly specialised procedure involving injecting a sclerosant solution into the abnormal veins using ultrasound guidance, causing the vein wall to collapse. The veins dissolve and disappear as the body gradually absorbs them.
Radiofrequency Ablation
Radiofrequency ablation (RFA) relies on thermal (heat based) damage to the vein, that leads to immediate closure of the vein. Once the vein is treated by radiofrequency ablation, it will gradually undergo complete absorption by the body and disappear over time.
Ambulatory Phlebectomy
Ambulatory Phlebectomy is the surgical removal of visible varicose veins, through keyhole incision. The procedure eliminates varicose veins through a series of small punctures (as tiny as 1mm) made in the skin adjacent to the vein.
Severe Varicose Veins
Before & After
View other Before and Afters for: Spider Veins | Periorbital Veins
Medicare Rebate & Costs
The cost of treating varicose veins depends on severity of the veins as well as which treatment is used. We discuss these costs in detail at your initial consultation.
A Medicare rebate is claimable on all varicose vein procedures, except the most superficial spider veins.

What to expect
Learn all about your first appointment, what's included, and how much it will cost.



