Chronic Venous Insufficiency (CVI) is when the leg veins can’t efficiently return blood to the heart due to valve problems, causing pooling, swelling, discomfort, skin changes, and sometimes ulcers. Early diagnosis and treatment (compression, minimally invasive procedures) can relieve symptoms and prevent complications.
If your legs often feel heavy, achy, or swollen — especially toward the end of the day — it could be more than just fatigue. These are common symptoms of Chronic Venous Insufficiency (CVI), a condition that affects the way blood flows through the veins in your legs.
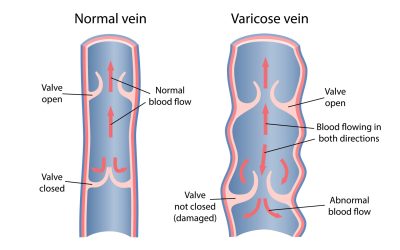
CVI occurs when the valves inside your leg veins become weakened or damaged. These valves are meant to keep blood flowing upward toward the heart, but when they stop working properly, blood can pool in the lower legs. This backward flow is known as venous reflux, and over time, it leads to venous hypertension — increased pressure in the veins that causes inflammation, skin changes, and in severe cases, ulcers.
What Causes CVI?
Chronic Venous Insufficiency often develops from longstanding or untreated varicose veins, where vein walls and valves gradually lose their function. Other contributing factors can include:
- A family history of venous disease
- Standing or sitting for long periods
- Hormonal changes from pregnancy
- Ageing and loss of vein elasticity
- Obesity or inactivity
How Do I Know If I Have Chronic Venous Insufficiency?
Symptoms usually start subtly and worsen over time. You might notice:
- A heavy or tired sensation in your legs
- Swelling around the ankles
- Itching or skin irritation
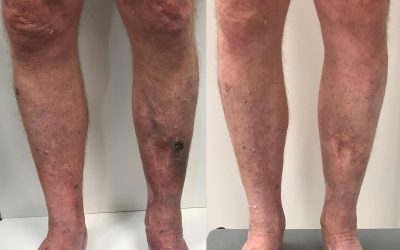
- Skin that becomes darker, leathery, or inflamed
- The appearance of visible or bulging veins
- In more advanced cases, open sores or venous leg ulcers
Many people ignore these signs for years, assuming they’re just part of ageing. But CVI is a progressive condition — it rarely improves on its own and can lead to serious complications if left untreated.
“Untreated CVI can lead to chronic pain, skin breakdown, and stubborn leg ulcers. These complications don’t just affect comfort — they can significantly reduce quality of life,” says Dr Peter Paraskevas, founder of Vein Health Medical Clinic. “That’s why early diagnosis and treatment are so important.”
Dr Paraskevas is a leading Australian phlebologist who has dedicated his career to treating venous disease and training the next generation of vein specialists. His reputation is built on evidence-based care, meticulous ultrasound diagnostics, and personalised treatment plans.
How Is Chronic Venous Insufficiency Treated?
The good news is that CVI can be managed — and often reversed — with the right treatment.
At Vein Health, we use advanced, minimally invasive techniques designed to shut down faulty veins and restore proper circulation. These include:
- Endovenous Laser Ablation (EVLA) – a laser fibre is inserted into the vein to seal it closed
- Ultrasound-Guided Sclerotherapy – a medical solution is injected to close off diseased veins
- Compression therapy – supports the veins and helps manage symptoms
All treatments begin with a comprehensive duplex ultrasound scan to map your veins and identify the source of reflux.
Is It Serious?
While early CVI may only cause mild discomfort, it should never be dismissed as a cosmetic issue. Left untreated, the pressure buildup in the veins can lead to irreversible skin damage, venous eczema, bleeding veins, and chronic leg ulcers that are painful and difficult to heal.
Key Takeaways
- CVI is a common and progressive condition caused by poor blood flow in the leg veins
- Symptoms include leg swelling, heaviness, itching, skin changes and ulcers
- If untreated, CVI can lead to serious complications like chronic wounds and skin breakdown
- Treatments are safe, walk-in procedures with minimal downtime
- A specialist ultrasound is essential for accurate diagnosis and treatment planning
Remember, following these guidelines helps ensure optimal results from your vein treatment and promotes long-term vein health. Every patient’s recovery journey is unique, so always follow the specific advice provided by your treating phlebologist.